

Together, let’s transform how care is delivered, managed, and paid.
Together, we work with clients across the healthcare ecosystem to meet their current and dynamic business challenges.
We help payers improve members’ care quality and network performance, manage population risk, and optimise revenue while decreasing administrative waste and reducing health claim expenditures.
We help provider organizations proactively manage risk, improve quality outcomes, optimize network performance, and drive member experience.
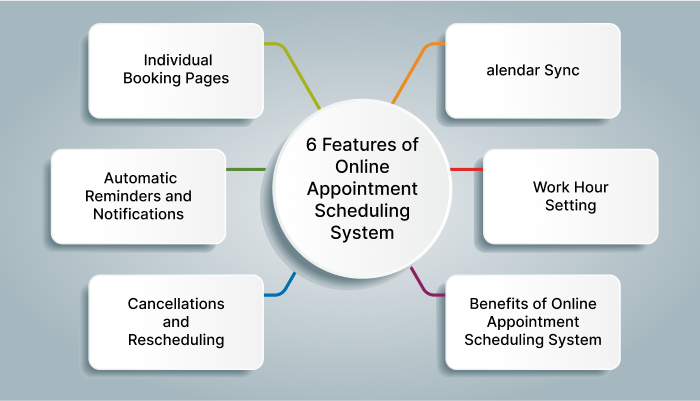
Patient Scheduling and Appointment Management services are designed to help healthcare providers manage their schedules more effectively while improving patient satisfaction. Our services include:
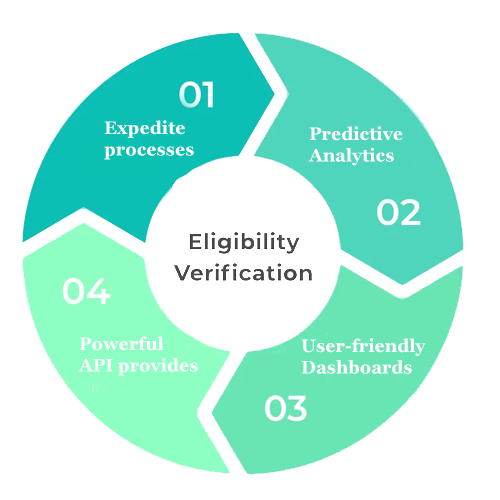
Our skilled team of experts handles the patient’s eligibility verification process. They have the expertise in confirming the patient’s coverage and benefits from individual payer websites and making phone calls. Our services include:
Establishing a clear and standardized process for collecting patient demographic information helps safeguard against critical mistakes being made at an early juncture.
We update the following patient information on the system:
Our charge entry transactions remain consistent throughout:
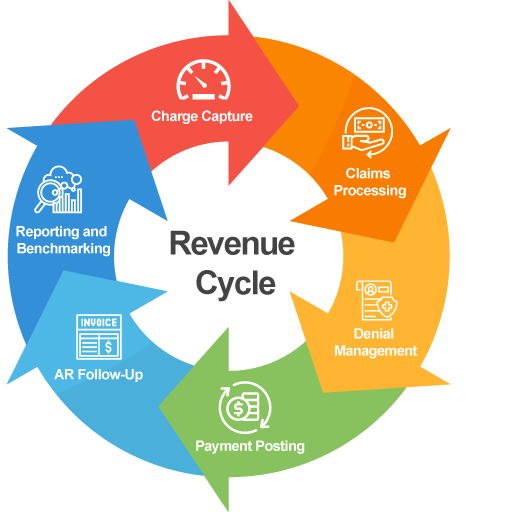

We process the following types of remittance transactions:
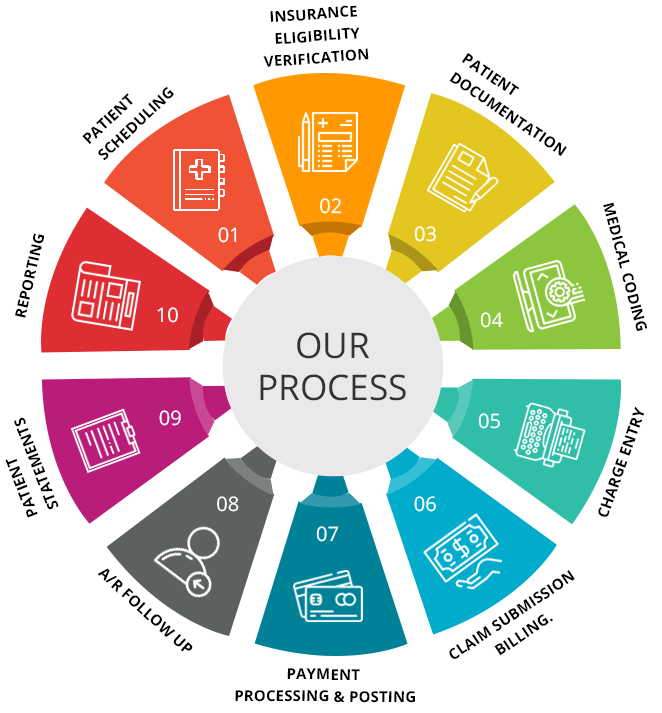
Accounts receivable (AR) teams are responsible for identifying outstanding balances owed to a provider and taking all necessary steps to ensure that payment is made. AR teams identify outstanding accounts, review them to discover why payment was never made, amend claim errors to resubmit them for payment, and collect from insurers or patients.
